At a Glance
- Medical colleges in India nearly doubled in the last decade.
- In Budget 2025, the Finance Minister announced to add 75,000 new MBBS seats in the next 5 years.
- But India has more than 30% of faculty vacancies.
- The rural-urban gap is not expected to reduce soon.
- Hard government decision and tough NMC compliance is the need of the hour.
India’s medical education has witnessed exponential growth in the past decade, with the number of medical colleges rising from 387 in 2014 to 780+ by 2025. While this surge in MBBS, postgraduate (PG), and super-specialty seats is commendable, it raises critical questions about the capacity of institutions, particularly teaching faculty and infrastructure, to maintain educational standards.
This article presents a data-driven comparison of government and private medical colleges in India, examining faculty strength, academic facilities, hospital infrastructure, and challenges across rural and urban settings.
Expansion of Medical Education: MBBS, PG, and Super-specialty Seats
India currently has over 118,000 MBBS seats, with roughly 50% in government colleges. PG (MD/MS) seats have surged to 72,627, and super-specialty programs offer nearly 5,000 seats. However, nearly 20% of super-specialty seats remain vacant due to low demand or poor training infrastructure, especially in newer or rural private colleges.
Many new government colleges have been created via centrally sponsored schemes (e.g. 157 new colleges by upgrading district hospitals, 109 already functional), often in underserved/rural regions. However, these rapid expansions have strained both staffing and facilities.
Teaching Faculty: Norms, Shortages, and Compliance
Both public and private colleges face severe faculty shortfalls. A NITI Aayog analysis found that by NMC norms, India needed about 138,028 teachers for 602 colleges, but only 96,649 were on record, ~30% nationwide vacancy.
Shortages are worst at junior levels: one study found ~40% vacancies among Assistant/Associate Professors (inverse “pyramid” with more Professors than junior faculty). Frequent causes include delayed recruitments, relocation preferences (urban bias), and inflexible rules (e.g. NMC’s 2019 ban on PG holders as basic-science faculty).
NMC mandates a strict faculty-to-student ratio and hierarchical distribution (Professor, Associate, Assistant Professors).
- Government Colleges
- Suffer from delayed recruitment, low incentives for rural postings, and retirement-age attrition.
- Tamil Nadu’s inspections in 2025 showed up to 95% departmental vacancies in many government colleges.
- Private Colleges
- Frequent reports of “ghost faculty” and under-qualified hires.
- A 2023 NMC audit found over 60% of private colleges violating attendance and teaching norms.
- Reforms & Suggestions
- Recent NMC relaxations allow retired or adjunct faculty, raise the retirement age to 70, and permit clinicians without teaching experience in certain roles.
- However, enforcement remains weak.
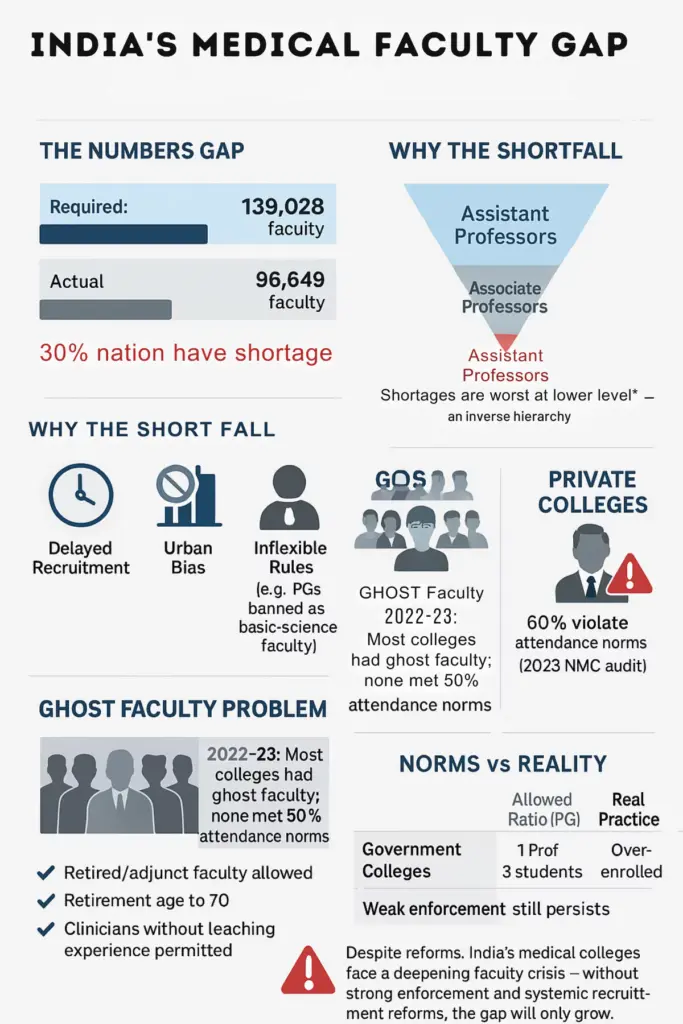
“Ghost faculty” (nominal staff who do not teach) is pervasive: NMC found in 2022–23 that a majority of assessed colleges (both public and private) had ghost faculty, and none met even 50% attendance requirements.
NMC norms set strict teacher-to-student ratios. For PG broad specialties, for instance, a government college Professor/Associate-Prof may have at most 3 students per year (1:3), whereas longstanding private colleges allow 2:1.
In practice, many colleges violate these norms simply by lacking staff or over-enrolling. Regulatory changes in 2025 have tried to ease requirements (e.g. allowing experienced clinicians as adjunct faculty and raising retirement age to 70) to fill gaps.
Still, the net effect is an acute shortage: with tens of thousands of vacant teaching positions, actual faculty-to-student ratios are far worse than required.
Academic Infrastructure: Classroom, Labs, and Digital Tools
Medical colleges are required by NMC to provide extensive academic facilities: multiple lecture halls (often convertible to digital “smart” classrooms), fully equipped laboratories for each pre-clinical and para-clinical subject, an anatomy dissection hall (typically ~250–400 sq.m for 200 students), museums, skill labs (for clinical skills training), and simulation centers.
New colleges are also urged to use e-learning systems. In recent expansions, many colleges have built modern facilities – for example, newly founded colleges often include simulation-based training centers and advanced digital classrooms.
However, audits frequently uncover deficits. In the Bathinda example above, inspectors found even the basics missing: anatomy tables were idle and “the dissection hall was not functional”.
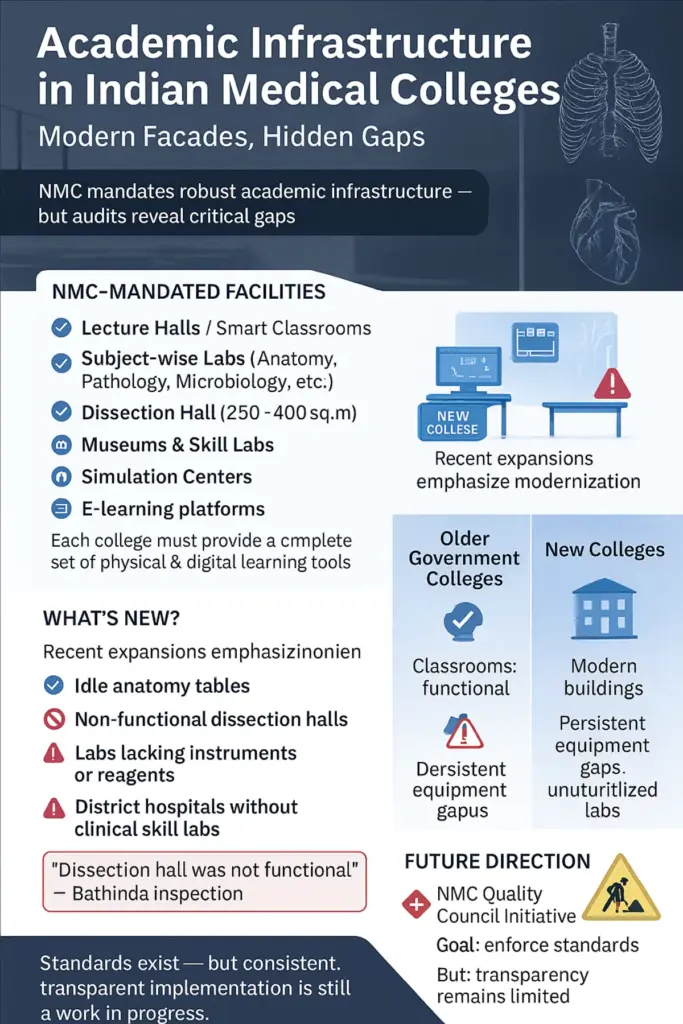
Similarly, clinical skills labs and equipment in district hospitals (now colleges) are often incomplete or underused. Pre- and para-clinical laboratories (chemistry, microbiology, pathology, etc.) sometimes lack instruments or reagents, forcing sharing or outsourcing.
Older government colleges often have adequate classrooms but ageing equipment. Many new colleges have built infrastructure to meet norms, but ongoing deficiencies are reported.
The NMC’s Quality Council rating initiative (starting 2024–25) aims to enforce standards, but transparency remains limited.
Hospital Infrastructure: Patient Load, Bed Strength, and Exposure
Medical colleges must have attached teaching hospitals with minimum bed strengths (at least 300 beds for a 150-seat college, 500 beds for 200 seats, 1000 for 250 seats under past norms), plus dedicated ICU, NICU/PICU, operating theatres, etc.
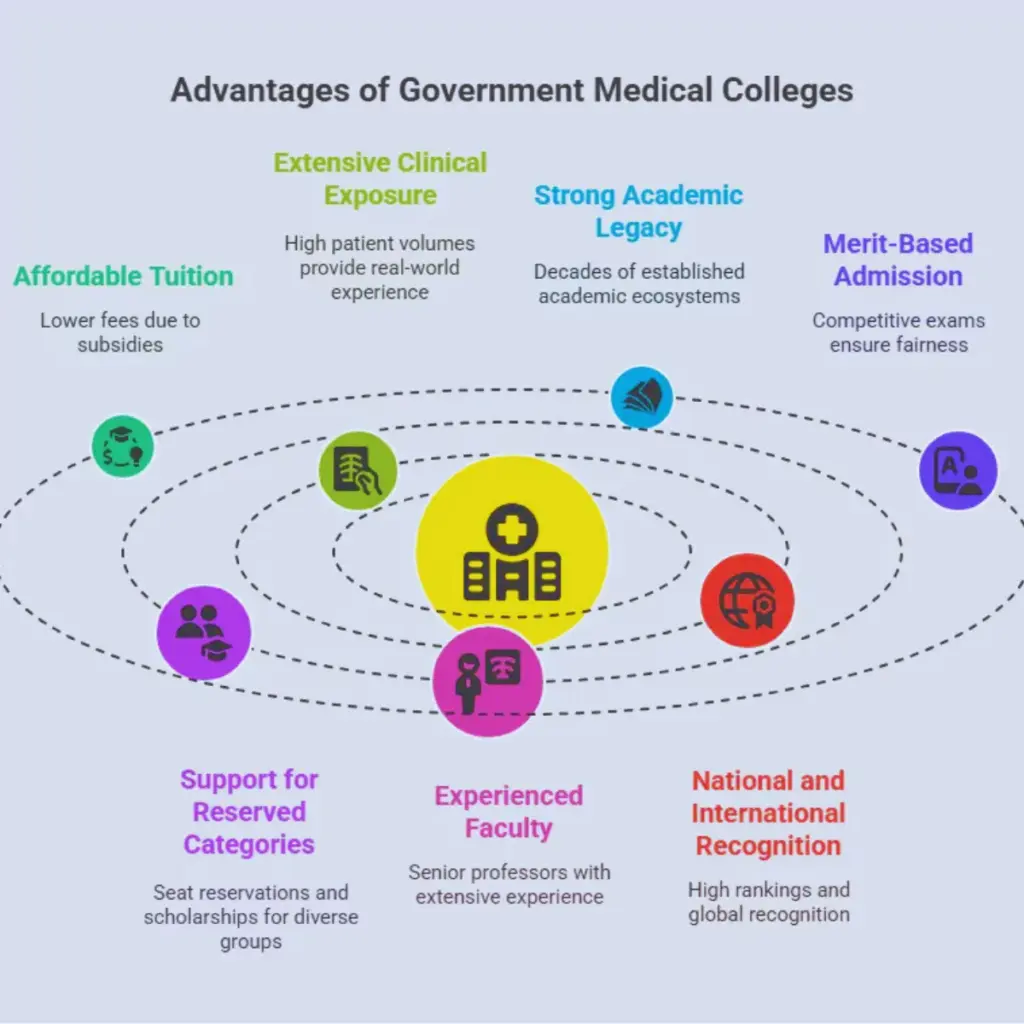
Government colleges typically meet these bed targets, but actual utilisation varies. Busy urban teaching hospitals see huge patient volumes, e.g. Kolkata’s five government college hospitals each see 5,000–8,000 OPD patients daily (pre-COVID).
This high footfall ensures student exposure and reveals staff shortages: when these hospitals temporarily shut OPDs, volumes plummet (as one report showed RG Kar College OPD dropped from 6,000 to 364/day).
In contrast, many private and rural colleges struggle to attract students.
In practical terms, government hospitals generally have very high bed occupancy (often >100%) and busy OTs/ICUs, whereas private college hospitals – especially in smaller cities – may see patchy utilisation. Some private colleges mitigate this by affiliating with corporate hospitals, but many rely on their in-house hospital.
Government vs Private Medical Colleges in India
Government Medical Colleges: Strengths and Weaknesses
- Strengths:
- Generally older and more established.
- Benefit from high patient inflow, ensuring robust clinical exposure for MBBS students.
- Weaknesses:
- Struggle with bureaucratic inefficiencies in hiring processes.
- Infrastructure often outdated, with slow upgrades.
- Even reputed government institutions are under scrutiny:
- In Tamil Nadu, the NMC issued show-cause notices to 34 of 36 government medical colleges due to faculty shortages and infrastructure gaps.
- Similar warnings were sent to states like Telangana and TN, urging urgent upgrades and staffing.
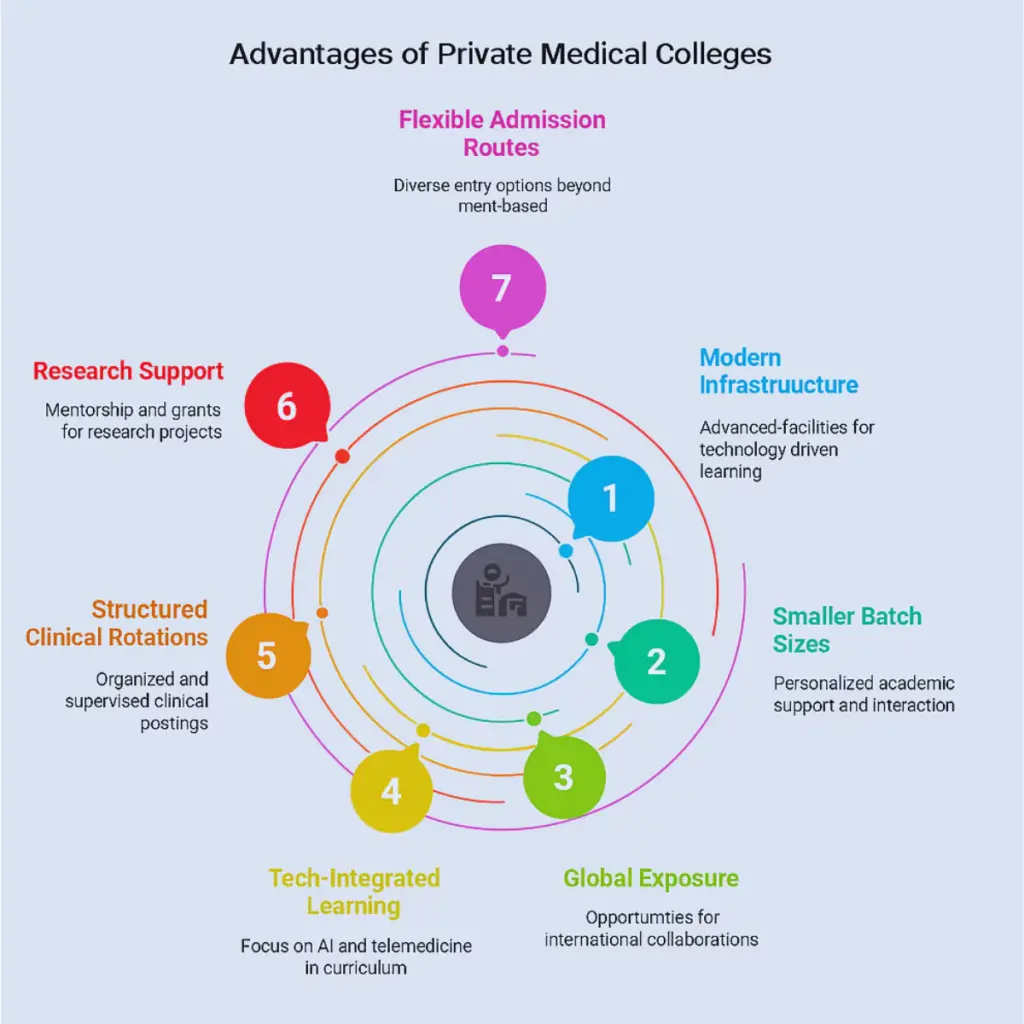
Private Medical Colleges
- Top-Tier Private Colleges:
- Some match or exceed government hospitals in modern infrastructure and simulation labs.
- Attract well-qualified faculty and international collaborations.
- Second-Tier and Newer Colleges:
- Often cut corners on staffing, hospital facilities, and clinical services.
- Lack transparency and charge exorbitant fees.
- Multiple reports of corruption and non-compliance:
- A 2025 CBI-NMC investigation revealed that dozens of private colleges gained recognition by bribing officials, despite lacking basic facilities and qualified faculty.
- The Adesh University (Bathinda) case is a notable example where severe infrastructure and clinical deficiencies led to derecognition by the MCI.
Systemic Oversight Failures
- Uneven Regulatory Enforcement:
- In 2023, only 246 of ~700 private colleges underwent assessment for renewal of recognition, leaving many uninspected.
- Many private institutions bypass scrutiny, especially post-initial recognition.
- Transparency Gaps:
- Self-Assessment Reports and internal audit data often remain unpublished.
- Despite multiple orders from the Chief Information Commissioner, the NMC has not released the mandated documents.
Geographic Disparities in Indian Medical Education
Regional Imbalance
- Western and Southern States (e.g. Karnataka, Tamil Nadu, Maharashtra):
- Well-established medical infrastructure with multiple colleges.
- Eastern and Northeastern States:
- Still underserved with limited access to quality medical education.
Urban-Rural Divide
- Urban Centers:
- Reputed hospitals with high patient loads.
- Rural/Tier-2 Colleges:
- Struggle with low patient footfall, faculty shortages, and limited clinical material.
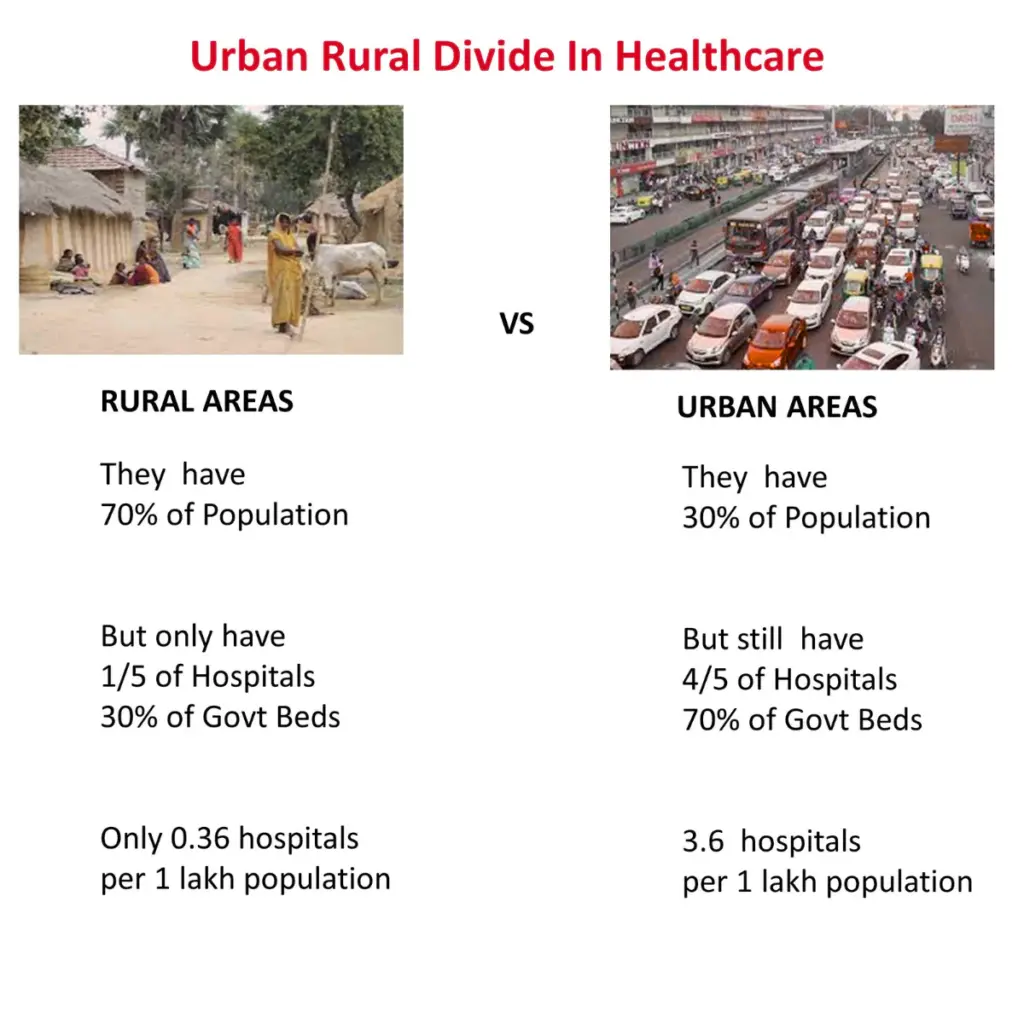
Rural College Challenges
- 109 new rural colleges under the upgradation scheme now face:
- Empty hospital wards,
- Unfilled teaching and medical posts,
- Failure to meet NMC’s 75% bed occupancy norm (e.g. in Haryana, Odisha).
Infrastructure vs. Functionality
- Private Tier-2 Colleges:
- Infrastructure is often built for show.
- Real teaching suffers due to lack of junior faculty or operational hospital units.
- Government Colleges:
- Bureaucratic rigidity prevents flexible faculty deployment to rural areas.
Policy Pressure & Quality Risks
- COVID backlog + 75,000-seat expansion plan = increased strain.
- 2025 NMC rule relaxation intended to boost capacity, but may compromise quality.
Key Recommendations to Improve Medical Education Infrastructure and Quality in India
Strengthen Faculty Recruitment & Retention
- Expand National Talent Pipeline
- Use NExT/NET-based scholarships to attract medical postgraduates into teaching.
- Incentivise Rural Postings
- Offer hardship allowances, housing, or scholarships for faculty children in rural areas.
- Utilise Adjunct Faculty
- Allow retired clinicians and non-teaching specialists to mentor in underserved colleges (per NMC 2024 norms).
- Ensure Attendance and Transparency
- Use AEBAS for biometric tracking and penalise absentee “ghost” faculty.
- Mandate private colleges to publicly display updated faculty lists and attendance logs.
Invest in Clinical Infrastructure
- Ensure Core Service Delivery
- Set and enforce minimum occupancy standards for OPD/IPD and critical departments.
- Referral & Outreach Networks
- Link district colleges to the surrounding PHCs for better patient flow.
- Encourage mobile clinics and telehealth programs to raise rural OPD volume.
- Utilise Full Capacity
- Activate underused ICU/NICU beds through tech-enabled referrals.
- Tie Performance to Recognition
- Private colleges with <70% occupancy or weak OPD/IPD load should face seat reduction or derecognition.
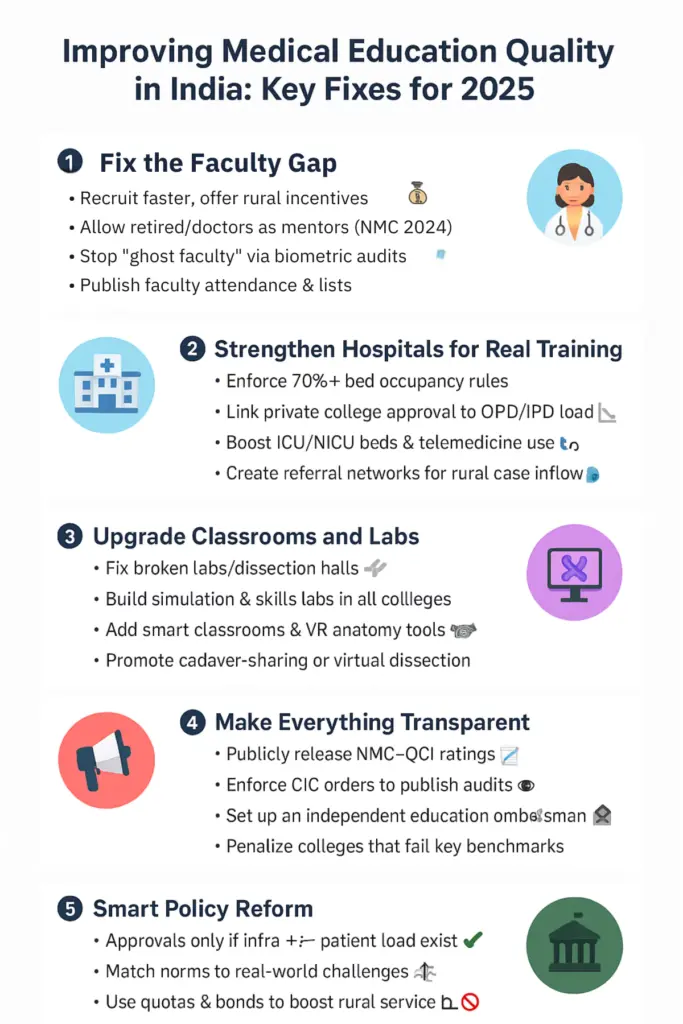
Upgrade Academic Facilities
- Enhance Teaching Infrastructure
- Fund dissection halls, skill labs, and simulation centers via state/central schemes or PPPs.
- Enforce Periodic Audits
- Penalise colleges with non-functional labs or neglected equipment.
- Promote Digital Learning
- Introduce smart classrooms and compulsory use of verified online platforms.
- Encourage Inter-Institutional Support
- Facilitate tele-cadaver or simulation-sharing between rural and urban colleges.
Improve Transparency & Accountability
- Public Access to Data
- Enforce CIC orders to publish Self-Assessment Reports and third-party audits.
- Make the NMC–QCI institutional ratings public every year.
- Independent Oversight
- Set up a medical education ombudsman for grievance redressal and compliance enforcement.
- Enforce Penalties for Non-Compliance
- Derecognize colleges with persistent faculty shortfalls (>10%) or poor bed occupancy (<70%).
Implement Policy & Regulatory Reforms
- Focus on Strengthening Existing Colleges
- Pair the freeze on new colleges with mandatory infrastructure and faculty upgrades.
- Revise Faculty Norms Thoughtfully
- Allow BSc-Med/MBBS-hybrid educators with oversight for foundational subjects.
- Reform Quota-Based Postings
- Link bonded rural service with proper incentives and support.
- Cautious Seat Expansion
- New seat approvals should be conditional upon compliance with NMC standards for faculty, infrastructure, and patient load.
Only expanding MBBS seats without matching investments in teaching faculty, infrastructure, and patient access will not suffice.
A data-driven, enforcement-focused approach is essential to bridge gaps between rural vs. urban and public vs. private medical institutions, ultimately improving health outcomes and educational quality nationwide.
India’s bold expansion in medical education must be matched by proportional investments in faculty and infrastructure. While both government and private colleges face serious challenges, issues like ghost staffing, low patient loads, and non-functional facilities are more prevalent in private institutions.
Targeted reforms, transparent governance, and digital innovations can bridge these gaps, ensuring that the country produces not just more doctors but better-trained ones for a future-ready healthcare system.