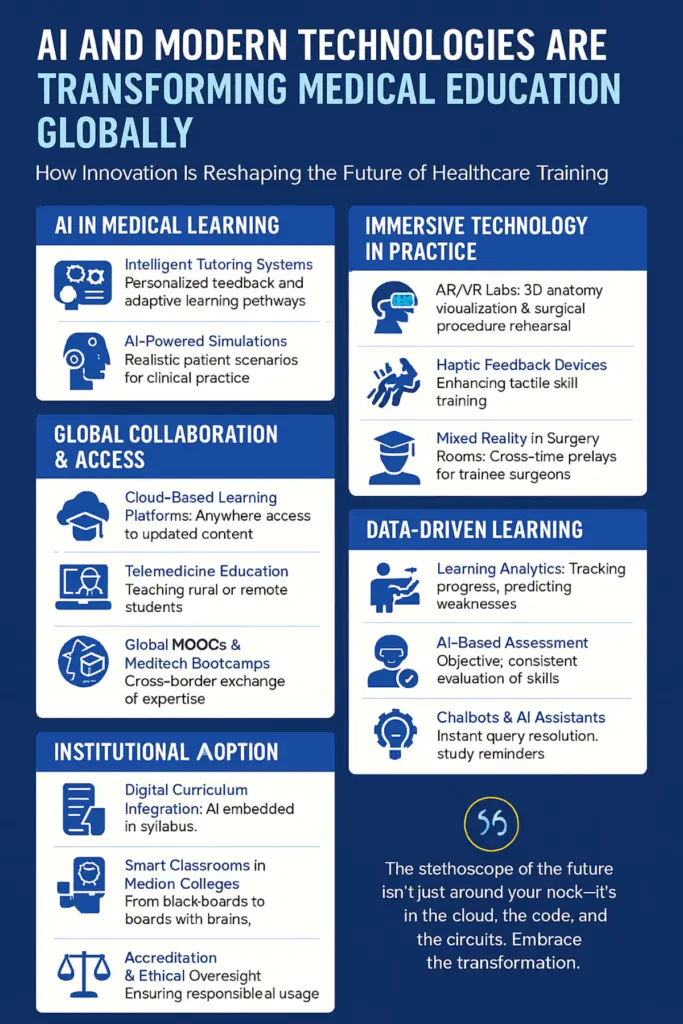
Medical education and training are rapidly incorporating AI and digital tools. New technologies include AI-powered tutors (chatbots and adaptive quizzes), virtual/augmented reality (VR/AR) simulations, robotic patient simulators, and digital anatomy platforms. Top institutions (e.g. Harvard, Stanford, Oxford) report pilot programs using these tools.
Benefits include personalised learning, enhanced clinical reasoning, and safer hands-on practice. However, challenges like infrastructure gaps, costs, ethical concerns (data bias, privacy), and faculty training remain, especially in low-resource settings. Looking ahead, experts predict even more immersive AI and AR experiences – e.g. haptic VR surgery training and AI-driven virtual patients – reshaping curricula, assessments, and doctor–patient communication training.
Stakeholders should invest in infrastructure and training, develop balanced curricula with AI literacy, and ensure equitable access and ethical use of these technologies.
AI and Modern Technology in Medical Education
AI-Powered Tutors and Chatbots
Modern large language models (LLMs) like GPT have been adapted to tutoring roles. For example, a 2025 study describes an AI “tutor” using an LLM to help students practice clinical reasoning with personalised cases and feedback. Many medical schools experiment with chatbot assistants (e.g. Khanmigo) or custom AI quizzes to deliver on-demand Q&A and explanations.
These systems can track student performance and adjust question difficulty, effectively personalising learning and helping students master complex topics at their own pace.
Virtual and Augmented Reality (VR/AR) Simulations
VR headsets and AR devices immerse learners in realistic medical scenarios. For example, VR can recreate an emergency department or a surgical suite in three dimensions, letting students “treat” virtual patients interactively. Such simulations overcome limits of traditional teaching by allowing repeated practice without risk to real patients. Studies note VR “can simulate the real clinical situation, stimulate enthusiasm…, and promote medical safety”. AR tools (e.g. holographic anatomy overlays) similarly let students explore anatomy or procedures in situ.

Virtual reality (VR) and augmented reality (AR) systems are increasingly used to create immersive medical simulations. VR can simulate real clinical environments and procedures, helping students learn by doing in a risk-free setting.
For instance, one review notes VR’s ability to simulate real scenarios and enhance learning engagement. These tools allow practice of complex clinical situations repeatedly, improving readiness for real-life cases without the pressure or danger of live patients.
Robotic Simulators
Humanoid and robotic “patient” simulators are used for hands-on practice. Recent research describes robots that present realistic symptoms (facial expressions, heartbeats, etc.) so trainees can conduct exams as if with real patients.
In one study, 67% of medical learners said they would use a humanoid robotic patient for diagnostic training in addition to actor-standardised patients; many appreciated being able to repeat case scenarios at their own pace.
Robots can deliver standardised cues (e.g. pulses, speech) and record performance metrics. This makes procedural training more consistent and repeatable: trainees can practice exam or bedside skills multiple times independently, improving their confidence before working with real patients.
Digital Anatomy Platforms and Online Resources
3D anatomy and virtual dissection tools (like Complete Anatomy or Visible Body) supplement or replace cadaver labs. These platforms let students manipulate highly detailed 3D models of the human body.
Studies note that digital anatomy has “revolutionised undergraduate anatomy education via 3D reconstruction”. In practice, many medical programs now give students app access to these models for studying outside the lab.
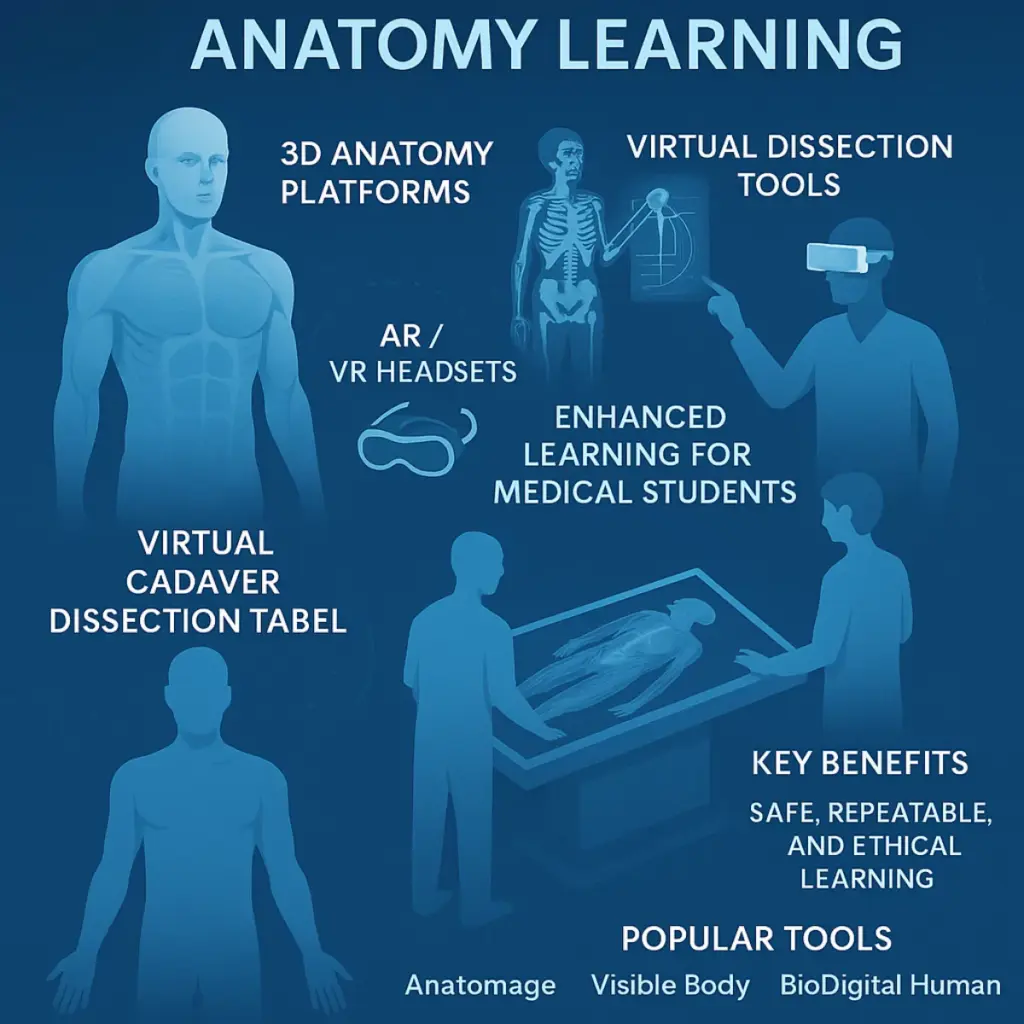
For example, during the COVID lockdown, students at one medical school received free access to a popular 3D anatomy app and reported high engagement because the app was easily accessible anytime. By comparison, access to an on-campus dissection table was more limited.
These digital tools reinforce spatial understanding of anatomy and allow interactive quizzes and virtual dissections in ways that static textbooks cannot.
Case Studies and Examples
Harvard Medical School (USA)
Harvard has begun integrating AI into its curriculum. For instance, incoming students take a month-long course on AI and machine learning in healthcare. The school also launched a PhD track in AI in Medicine, reflecting strong interest (400 applicants for 7 spots).
The HMS curriculum now encourages students to use AI tools (like GPT) as study aids. This proactive approach aims to prepare doctors who understand AI’s power and pitfalls, rather than banning it. (By late 2024, ChatGPT had passed the USMLE licensing exam, highlighting AI’s level of performance.)
Stanford University (USA)
Stanford’s neurosurgery department uses VR extensively. One VR system lets residents walk inside a patient’s 3D brain scan before surgery. Surgeons can practice on the model and plan approaches in virtual space.
Stanford reports that the 3D visualisation “eases surgeons’ planning and improves accuracy,” ultimately making procedures safer. VR is also used to educate patients by showing them their own anatomy.
Furthermore, Stanford doctors are experimenting with AR headsets (e.g. Apple Vision Pro) to overlay imaging data onto their field of view during operations.
Imperial College London (UK)
Imperial developed immersive VR simulations for its medical curriculum. In a notable program, all Imperial medical students don VR headsets for emergency scenario training (e.g. cardiac arrest, severe asthma).
The students reported that these scenarios felt “incredibly real”, allowing them to apply textbook knowledge to life-threatening cases in a safe “virtual ward”. The school has integrated these VR exercises into its official MBBS curriculum and is rolling them out more broadly via the NHS.
According to faculty, this gives every student exposure to core emergencies in a consistent way, addressing gaps from unpredictable ward teaching.
University of Oxford (UK)
Oxford’s anatomy department trialed a VR anatomy app (3D Organon) with its medical students. They provided students Oculus Quest headsets loaded with the app during anatomy courses. Feedback was very positive: faculty noted that VR “breaks the complex barriers to understanding anatomical structures”.
In a survey of 65 students, the vast majority responded yes when asked if VR sessions should be part of future anatomy teaching. Students said seeing structures in 3D and interacting with them made learning more engaging and memorable.
Oxford plans to continue supporting such VR experiences alongside traditional methods, as a “promising way of teaching” anatomy.
All India Institutes of Medical Science (AIIMS, Delhi)
AIIMS and Wipro GE Healthcare Sign MoU to Establish ‘AI Health Innovations Hub’. IIT Delhi and AIIMS Delhi have launched a ₹330 crore Centre of Excellence to develop AI-driven healthcare solutions for national health challenges.
AIIMS Delhi, in collaboration with Microsoft Research and IIT Delhi, has pioneered the use of AI algorithms to:
- Detect lung nodules and brain tumors on CT/MRI scans.
- Triage high-risk emergency cases automatically.
- Use machine learning to predict patient outcomes in ICUs
Other Initiatives
Many other schools report similar efforts. For example, nursing faculties in the UK have built dedicated VR simulation suites for clinical training. Some hospitals and global organizations (e.g. Health Education England) are deploying VR across regions to standardize training.
In low-income countries, pilot projects are using low-cost mobile-VR setups to scale up life-saving skills training where full simulation labs are not available. These diverse examples illustrate how top institutions are embracing technology to enrich medical education.
Benefits for Faculties and Students
Enhanced Learning and Retention
Immersive and interactive tools improve understanding. Studies show medical students achieve higher knowledge gains using immersive VR than with traditional screen-based or lecture methods.
VR simulators have been widely adopted in surgical training because they allow practice in a risk-free environment; research finds VR-trained surgeons make fewer errors and perform procedures faster than untrained peers.
AI tutors and adaptive platforms similarly boost engagement and recall by tailoring content to each student’s level.
Improved Clinical Reasoning
Simulation tools sharpen decision-making. In VR scenarios, learners gather history, order tests, and make diagnoses in real time, then receive automated feedback on their choices. This deliberate practice helps bridge theory and real-life thinking.
In one pilot project, students appreciated how a VR code-blue scenario let them “work with [the] team to save the patient” without any real risk.
Similarly, AI-driven case drills (chatbot patients) let students repeatedly practice clinical reasoning questions, which enhances diagnostic skills over time.
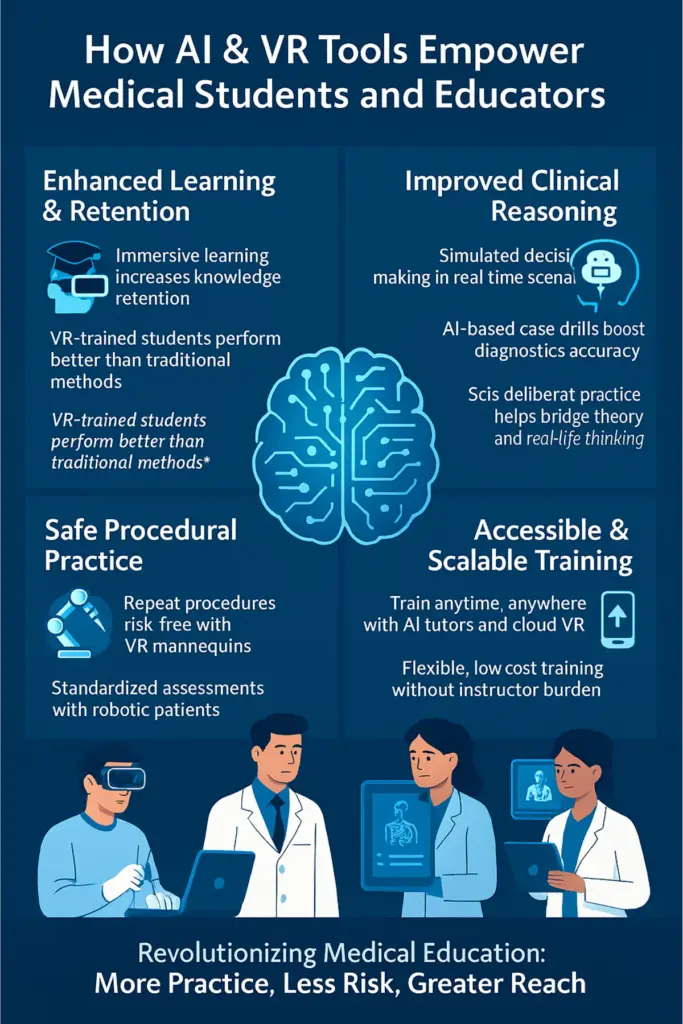
Safe Procedural Practice
Hands-on simulators (robotic patients or VR mannequins) enable repetitive practice of physical exams and procedures. Learners can make mistakes on a virtual patient or robot as many times as needed.
For example, robotic simulators standardise the patient interaction so that each student confronts the same scenario, allowing objective assessment of skills.
Evidence shows that such practice builds confidence: in one study, 67% of trainees said they would use a humanoid simulation in addition to video cases, valuing the ability to repeat cases at their own pace.
Importantly, VR-based nursing simulations were found to yield equivalent skill acquisition as manikin-based labs, but at significantly lower cost.
Accessible and Scalable Training
Digital tools break traditional constraints. A VR setup can serve many students with minimal faculty overhead: some systems require little instructor presence, letting students run scenarios independently and then discuss feedback.
Similarly, AI tutors can be accessed anytime for self-directed learning. This makes training more flexible (like “going to the gym” when ready) instead of once-in-a-while workshops.
Especially in resource-limited settings, mobile VR or cloud platforms can deliver content without expensive labs. And in ongoing medical education, these tools allow clinicians to refresh skills remotely, making continuous training more practical.
Overall, technologies can expand reach and frequency of training while saving faculty time and physical resources.
Ethical and Infrastructure Challenges
Access and Infrastructure
A recent review notes that medical schools in low- and middle-income countries often do not have high-speed internet, cloud computing resources, or funds for expensive simulators.
Without these, cutting-edge AI and VR tools remain out of reach. Even in wealthier schools, budget constraints limit how many headsets or robots can be acquired.
Solutions like cloud-based AI or low-cost VR headsets are proposed, but inequities persist: institutions with deep pockets benefit most.
Training Faculties
Many faculty members need upskilling to effectively use these tools. The same review found that educators in resource-limited settings have little access to AI/tech training programs, leading to uneven adoption.
If teachers aren’t comfortable with a VR system or an AI tutor, it may sit unused. Thus, rolling out new tech requires dedicated faculty training and curricular integration; simply purchasing devices is not enough.
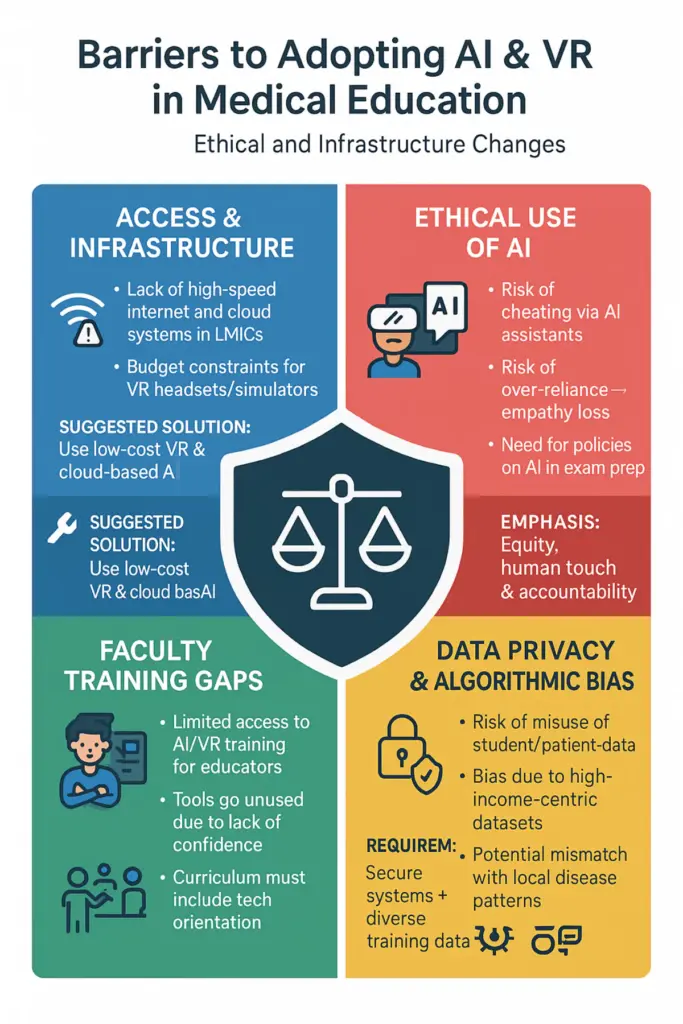
Data Privacy and Bias
AI tools rely on large datasets, raising privacy concerns. Student data (e.g. performance records) and patient data used to train algorithms must be secured. Ethical guidelines for AI in education are still evolving.
Moreover, most AI models are trained on data from high-income contexts; experts warn this can embed biases and reduce relevance in other settings. For example, an AI diagnostic simulator trained on Western patient data might not represent diseases common in Africa or Asia.
Without careful oversight, such bias could mislead students. Medical educators stress the need for “human aspects” – ensuring AI supports patient-centred care rather than replacing it.
Students must be taught about AI’s limits: one review noted concerns that over-reliance on AI might erode empathy or clinical skills unless explicitly addressed in training.
Ethical Issue
As in any field, AI raises ethical issues. Automated assessment or chatbots could inadvertently promote cheating or diminish feedback if not monitored. There are debates about using generative AI (e.g. GPT) for exam prep: while it can guide learning, it could also be misused.
Clear policies are needed on acceptable use. Additionally, stakeholders must ensure technology doesn’t exacerbate disparities: giving privileged students AI tutors while poorer schools lag would widen gaps.
All these require thoughtful governance, data security, and an emphasis on equity.
Future Predictions
Looking ahead, experts predict even more sophisticated integrations:
AI-Powered Interactions
Virtual patient simulations will become more “alive” with AI. Researchers predict AI will make virtual patients behave and speak more realistically, and can analyze learner performance in depth.
For example, AI tutors could adapt cases on the fly to a student’s weaknesses or use natural language to hold complex patient interviews. Speech and voice recognition combined with VR could train communication skills in immersive role-plays.
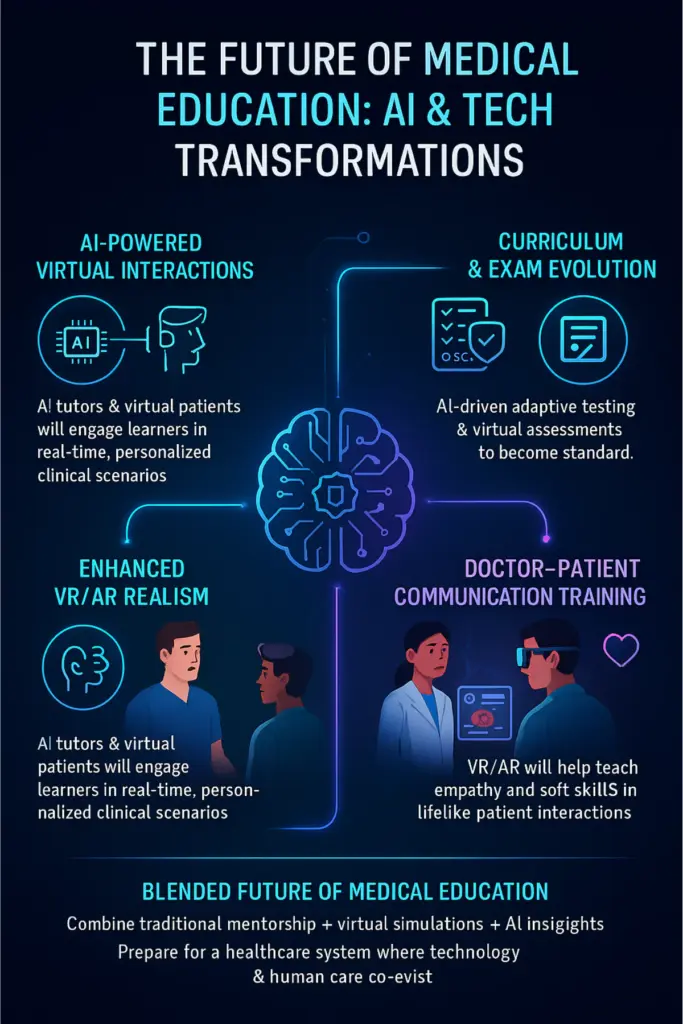
Enhanced VR/AR Realism
Hardware advances will blur the line between real and virtual. Improved haptic feedback devices (force-feedback instruments) and more natural hand/eye tracking are on the horizon.
This means future VR surgery simulators could provide realistic touch sensations, making skill transfer to actual surgery easier. AR glasses may overlay patient data during actual clinical encounters for training purposes.
Multiplayer VR experiences – already emerging – will allow geographically dispersed students to collaborate in the same virtual case, mirroring team-based care.
Curriculum and Exams
The medical curriculum will likely formally include AI and tech content. We expect standardised AI-literacy modules (teaching algorithm basics, biases, etc.) will be adopted, as well as greater use of digital exams.
Some medical schools are exploring VR-based assessments (virtual OSCEs) to safely test clinical skills. Adaptive testing, where AI evaluates students’ answers in real time, could replace some traditional exams, providing instant, personalised feedback.
Overall, the role of the teacher may shift from lecturing on facts to mentoring students in navigating data and technology-augmented care.
Doctor–Patient Communication Training
Future tech may use VR/AR to simulate patient encounters for soft-skills training. For instance, a student in VR could interview an AI-driven virtual patient who expresses emotions and reactions.
These “digital standardised patients” could provide a safe rehearsal of breaking bad news or managing difficult conversations. Augmented reality might also be used in real clinics, training trainees how to overlay language translation or empathy cues in telemedicine.
In short, training for the human side of care will also be enhanced by these tools.
Overall, medical education is moving toward a blended future where AI and digital simulations complement traditional methods. The most forward-looking programs already combine live patient learning with virtual and AI experiences, preparing students for a healthcare landscape where technology and human judgment co-evolve.
Key Recommendations
Invest in Infrastructure
Governments and institutions should fund the needed hardware and connectivity, especially in low-resource regions. This might include subsidising VR kits, upgrading broadband for schools, and providing cloud access. International partnerships (e.g. shared AI resources) can help bridge gaps.
Faculty Training and Support
Educators need training to effectively use new tools. Medical schools should offer workshops on VR simulation facilitation, AI literacy, and integrating tech into teaching plans. Pairing tech specialists with clinical faculty can ease this transition.
Curriculum Integration
Medical curricula must evolve to include AI and digital health competencies. This includes basic instruction on how AI works, its ethical pitfalls, and practical sessions using simulators. Accrediting bodies should consider adding AI/tech competencies to standards for medical graduates.
Ethical and Regulatory Frameworks
Policymakers and institutions should establish guidelines for data privacy and AI ethics in education. This includes ensuring patient data used in simulations is anonymised and that AI tools are validated for educational use. Clear policies on AI use in exams and assignments will safeguard fairness.
Equity and Accessibility
Stakeholders must proactively address the digital divide. For example, make sure learning platforms are mobile-friendly, support multiple languages, and are affordable. Scholarships or grants could help under-resourced schools adopt these innovations.
Research and Evaluation
Continue rigorous study of outcomes. Funding agencies should support research into the effectiveness of these technologies in various contexts. Sharing case studies and best practices (via conferences or publications) will help refine approaches.
Global Collaboration
Encourage international collaboration to share resources, such as open-source VR scenarios or multilingual AI tutors. Forums and consortia can help low- and high-resource institutions learn from each other’s experiences.
By following these recommendations, policymakers can harness AI and modern technology to produce better-trained doctors worldwide, while mitigating risks and ensuring that advances benefit all learners equally.